Disclaimer: The following blog post is written from my personal perspective as an individual with a mutation in the SDHB gene, which can lead to the development of paragangliomas. It is important to note that everyone’s experience with this genetic mutation and associated conditions may vary. The information provided aims to offer a general understanding of the topic and should not substitute professional medical advice. I strongly recommend consulting with a healthcare professional familiar with your specific situation for personalized guidance and treatment options.
What are Paragangliomas?
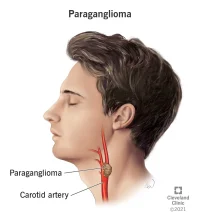
Paragangliomas are rare tumors that originate from specialized cells of the nervous system called paraganglia. These tumors most commonly form in the head, neck, and abdomen. Paragangliomas are unique because they arise from neuroendocrine cells, which release hormones into the bloodstream. As a result, these tumors can sometimes cause hormone imbalances.
Understanding the SDHB Gene Mutation
The SDHB gene, or succinate dehydrogenase complex iron sulfur subunit B gene, is responsible for providing instructions to produce a protein that plays a crucial role in the normal functioning of mitochondria. Mitochondria are the energy-producing structures within cells.
When a mutation occurs in the SDHB gene, it disrupts the production of the protein it encodes. This disruption affects the function of the mitochondria, leading to the development of paragangliomas. Mutations in the SDHB gene can be inherited from parents or can occur spontaneously in an individual’s genetic makeup.
In my case: According to the genetic testing conducted, my mutation is a spontaneous one. However, I have passed the mutation onto one of my children.
How Paragangliomas Develop
 The SDHB gene mutation can lead to the uncontrolled growth of paraganglia cells, resulting in the formation of tumors. These tumors can occur in various parts of the body, including the neck, abdomen, kidney, and areas around the heart.
The SDHB gene mutation can lead to the uncontrolled growth of paraganglia cells, resulting in the formation of tumors. These tumors can occur in various parts of the body, including the neck, abdomen, kidney, and areas around the heart.
Paragangliomas in the Neck: When paragangliomas develop in the neck, they are typically found along the carotid arteries or near the jugular vein. These tumors can cause symptoms such as a lump or swelling in the neck, difficulty swallowing, or changes in voice.
Paragangliomas in the Abdomen: Paragangliomas that form in the abdomen are often located near the adrenal glands, which produce hormones that regulate various bodily functions. Tumors in this region can cause abdominal pain, high blood pressure, or hormonal imbalances.
Paragangliomas near the Kidney and Heart: Tumors occurring near the kidney or behind the heart can be particularly challenging to treat due to their proximity to vital organs. Depending on their size and location, they may cause symptoms such as back pain, chest discomfort, or irregular heart rhythms.
Treatment and Management
Treatment options for paragangliomas vary depending on the size, location, and potential spread of the tumors. Surgical removal is often the primary approach, particularly for localized tumors. In some cases, radiation therapy or targeted drug therapy may be used to shrink or control tumor growth.
Due to the hereditary nature of SDHB gene mutations, individuals with this genetic mutation may require regular medical monitoring, including imaging tests, to detect any potential tumor development at an early stage. Managing hormone imbalances associated with paragangliomas may also require specialized medical care.
In My Case
So far, I have undergone several surgeries to remove paragangliomas from both sides of my neck, and one required radiation therapy. Additionally, I have had one paraganglioma removed from around my heart and another from around my kidney. as of my last checkup. the paragangliomas currently in my body have been stable since the previous scan which is good news.
Living With This
Living with a mutation in the SDHB gene that predisposes you to paragangliomas can be challenging. However, understanding the basics of this endocrine disease and the role of the SDHB gene can empower you to make informed decisions about your healthcare. Remember to consult with medical professionals experienced in managing paragangliomas to ensure appropriate monitoring and treatment for your condition.
In my long-term experience, I have encountered symptoms such as nerve damage in my neck, leading to paralysis in my face and throat. This paralysis has caused complications with swallowing, saliva generation, tongue movement/control, and swallowing control. Additionally, I have experience even today large fluctuations in my blood pressure due to the removal of one of my carotid bodies.
Please note that the above information is based on my personal journey and may not reflect the experiences of others.
